This spring, we are emerging from a year like no other. It has been one full year since NOSM University was proclaimed Canada’s first independent medical university, and here we are on the cusp of granting our first degrees as a university to MD graduates—a historic moment. In the last year, we also have established a new Board of Governors and a new Senate; we have made leadership changes to reflect our new status, hired our first Provost and in Sudbury, we will be installing our first Chancellor at convocation on Friday, May 26.
The shift to one convocation is a necessary one as, no matter where we all are in Northern Ontario, we are one university and one student body. Our ceremonies must reflect that unity, and bring us all together. It is also a legal requirement that the Chancellor grant the degrees at convocation, and so a unified event is essential. This year however, we also recognized that as a part of our transition it was important to have a commemorative event in Thunder Bay to celebrate the west campus. Both events will be available on our YouTube channel.
I believe that graduates of our programs are uniquely prepared to solve the challenging and ever-growing problems in health-care delivery in Canada, and will serve as transformational health-care leaders in our communities. We have reaffirmed through evaluation and accreditation reports that our focus on community, equity, diversity and inclusion, in concert with the outstanding team of staff, faculty and decanal leaders, have made NOSM University the best in Canada and highly-renowned in the world.
We are incredibly proud of our graduating students, who have shown exceptional flexibility, creativity, and resilience during their time with us. Many congratulations to the Class of 2023, our future leaders in health care, and the first class of NOSM University degree recipients (and our 15th class of graduates since 2009). This is an extraordinary time within academic and clinical medicine. There are so many opportunities to strengthen our health-care systems, address inequities in care, and promote the health of patients and populations. Be part of the solution. Your journey to reimagine, transform and disrupt the ways health care is delivered, especially with compassion and equity, is just beginning. I know you will succeed. Go full of hope to your new beginning and make it count. You, and our world, will be better for it.
At NOSM University, we will not rest on our laurels. We will strive to tackle the hard questions and lead in Canada. In fact, our success has been noted by several emerging medical schools, all calling us to find out the recipe for our ‘secret sauce.’ Truth be told, success is rooted in hard work. We have faced the pandemic, the insolvency of a major partner and an unprecedented expansion of our medical education programs. With hard work, we have prevailed.
I hope our newest alumni, and all of those who’ve shared this journey, can take the time to appreciate their accomplishments. As graduation approaches, we look forward to welcoming the class of 2023 to our alumni community. I sincerely hope—as you think of this year’s graduates and reflect on your future—you are able to rekindle the excitement of those moments that brought you to NOSM University and where they will lead you into the future.
Remember alumni: you will always have a home here at NOSM University. Stay in touch and come for a visit—or even better—come practise in Northern Ontario. We need you.
And now for more good news. As I announced on March 31, 2023, the government has announced funding for 100 new MD seats and 154 new PGME seats to be allocated across the province. This is in addition to the seats announced by Premier Ford last year.
Here is what this ultimately means for NOSM University:
- By 2028, through a gradual approach, we will offer a total of 108 MD seats, nearly doubling the capacity of our MD program.
- By 2028, we will almost double our postgraduate positions; this will be accomplished through the addition over the next five years of a commensurate number of positions for existing and new residency programs.
I heartily welcome this investment into medical education in Northern Ontario and am extremely supportive of the government’s expansion plans. This is fantastic news not only for the health-care landscape in the North, but also for the continued success of NOSM University.
My personal thanks go to our leaders in UME and PGME as they tackle this expansion; to the faculty, staff and stakeholders who support us; to our donors who are supporting and investing in our vision and our students; and, to the city councils and mayors across the region who continue to advocate for NOSM University: we are going to change the world.
Miigwetch, thank you, marsi, merci,
Dr. Sarita Verma
President, Vice Chancellor, Dean and CEO
NOSM University
If you have any feedback or comments, please reach out at president@nosm.ca and follow me on Twitter @ddsv3.
You’re Invited to join us Virtually for Convocation 2023!
NOSM University Achievement Celebration Honours Excellence in Medical Education

The accomplishments of faculty, learners and alumni—among the brightest in Canada—were celebrated at the inaugural NOSM University Achievement Celebration, held on Friday, May 5, 2023 in Thunder Bay. From among our exemplary community of scholars and learners, we are proud to acknowledge these recipients with the most extraordinary accomplishments this year.
Read more.

Federal Health Minister visits NOSM University
NOSM University was delighted to host the Federal Minister of Health, the Hon. Jean-Yves Duclos, on Tuesday, May 23, 2023. Minister Duclos was accompanied by federal MPs Viviane Lapointe (Sudbury), Marc Serre (Nickel Belt), and City of Greater Sudbury Mayor Paul Lefebvre (former MP). There were substantive discussions about health reform and health human resources, as well as the need for support for research infrastructure for smaller universities like NOSM University.
(Greater Sudbury Mayor Paul Lefebvre, Sudbury MP Viviane Lapointe, President Vice-Chancellor, Dean and CEO of NOSM University Dr. Sarita Verma, Nickel Belt MP Marc Serre, the Hon. Jean-Yves Duclos, Minister of Health.)
Upcoming Events
 Northern Health Research Conference
Northern Health Research Conference
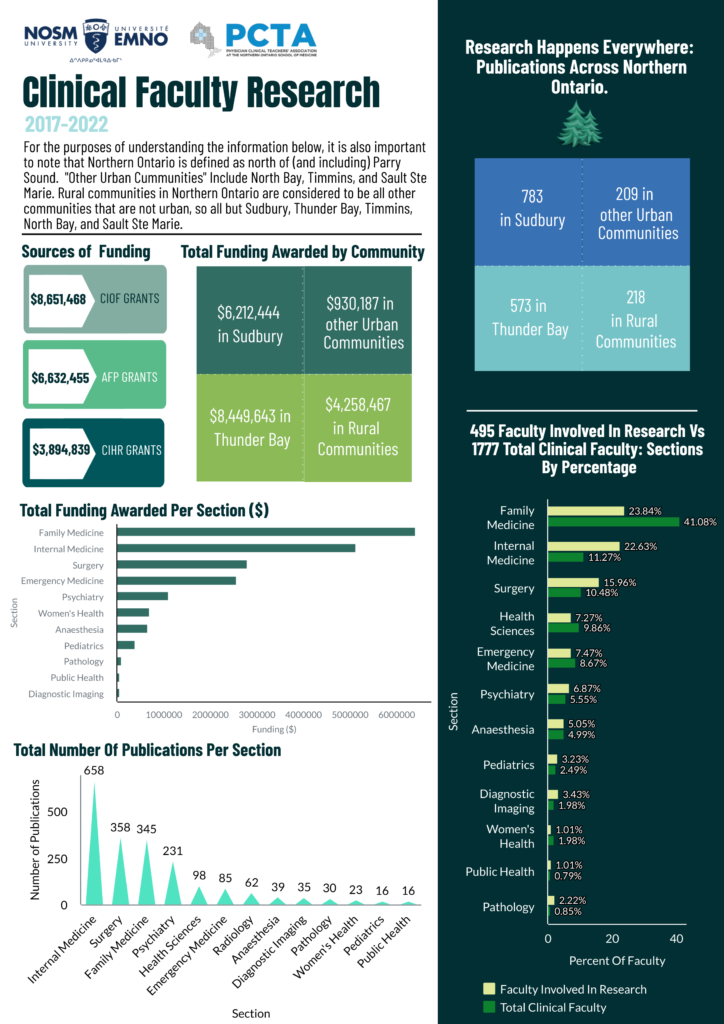
NOSM University will hold the 18th annual Northern Health Research Conference (NHRC) from Thursday, June 1 to Friday, June 2, 2023.
Held in Thunder Bay, the conference will be available in-person or online. This conference demonstrates NOSM University’s ongoing commitment to health care and education in Northern Ontario. Collaboration and community networking continues to be a significant force in the development of a culture of research activity. NHRC 2023 will feature a wide variety of oral and poster presentations related to NOSM University’s research priorities, which can be viewed at report.nosm.ca.
For more information, or to register for the NHRC, please email research@nosm.ca.



 Dr. Christopher Mushquash, NOSM University Professor, is the recipient of the very prestigious
Dr. Christopher Mushquash, NOSM University Professor, is the recipient of the very prestigious