Our Physician Workforce Strategy: NOSM Solutions
Posted on November 17, 2020
There is a serious physician workforce crisis looming in Ontario. The physician shortage has been influenced by several important factors that predate COVID-19, but the consequences of the pandemic have exacerbated the situation significantly. Some of the reasons for the physician shortage include:
- Disruptions for graduating physicians going into independent practice (provisional licenses are in place but time out for delayed exams);
- Early retirement of some physicians because of COVID-19 or changes in their scope of practice due to workload challenges;
- Ongoing difficulty in recruitment and retention for rural, northern, Indigenous and Francophone communities, and under-represented populations;
- Insufficient residency positions in Ontario, causing a net migration of newly-graduated MD’s out of the province; and,
- Some physicians decreasing the size of their practice to manage effectively the increasing needs of the population—in particular the population with complex, chronic illnesses.
The deficiency of physicians for historically underserviced and vulnerable populations has been an ongoing challenge. The current pandemic has been superimposed on an already fragile system and has exacerbated the concerns of care delivery sustainability. Specific areas of care such as mental health, public health, long-term care, and seniors’ care are particularly affected.
The pandemic has further highlighted for the Council of Ontario Faculties of Medicine (COFM) the urgent need for both a re-evaluation of the workforce pipeline and the comprehensive development of novel ways to achieve better distribution of physicians across the province. The six medical schools agree that we urgently need to reconcile the demographic needs of the province, practice patterns of the contemporary physician, and the future health-care needs of communities.
The current planning model is not sufficiently nimble to adjust to crises and major disruptions like COVID-19. System fragility and instability remains in many communities and is anticipated in others due to an aging/retiring physician workforce, an increased demand for patient care while at the same time having to train NOSM learners across Northern communities to obtain the necessary skills for clinical practice. Thus, COFM has submitted a proposal to expand all medical schools in undergrad and postgrad positions to increase the number of doctors in Ontario. NOSM is a full participant on this proposal.
An unpredictable and fragile Northern physician workforce.
Today, we are facing an unpredictable and fragile Northern physician workforce, with many clinicians on the brink of either retiring (aging physician workforce) or withdrawing from some services including teaching—an essential element of the NOSM distributed model—as clinicians continue to be under-resourced, overwhelmed and only able to focus on immediate patient care needs. This has been exacerbated by the COVID-19 pandemic changes in work commitments for clinicians. Those who remain in the Northern physician workforce are deeply worried and concerned that Northern Ontario is in the same crisis it was in when the original review of need made its recommendations 20 years ago.
Currently, physician shortages/vacancies across Northern Ontario exist as follows:
- > 100 family physicians – mostly rural generalists; and,
- > 100 specialists in the five Northern urban hospitals, but also in large rural communities like Sioux Lookout and Kenora.
Additionally, it is estimated (through work done recently by the Centre for Rural and Northern Health Research) that up to 50% of rural clinicians expect to retire in the next five years.
In relation to individuals in other areas of the province, in the North there is:
- lower life expectancy (by two years on average);
- greater difficulty accessing primary care in a timely way;
- increased burden of complex chronic conditions; and,
- greater burden of mental illness and addictions.
We are on it.
We are focusing on developing the best residency programs. There are new pathways being launched, including the Rural Generalist Pathway (RGP). The RGP is envisioned as a pathway with multiple points of entry from high school through to postgraduate training, culminating in an attractive clinical and academic career in a rural community, well-supported through meaningful contracts and administrative resources and ideally with a faculty designation that acknowledges the breadth of the Rural Generalist role.
The Rural Generalist faculty of NOSM will be supported to be “joined up” in ways that support mentorship, leadership, and resilience of the clinical community of rural Northern Ontario. We are deeply engaged in advocacy for recruitment and retention of physicians with our partner hospitals and Academic Health Science Centers. Our strategic plan focuses on our primary mandate—the strategic direction Transform Health Human Resource Planning means we are working on developing better data to identify the ‘needs of Northern Ontarians’ and the best ways to align the output of physicians to practicing in areas of need. Reforming our admissions process and criteria to curricular reform and improving community engagement are specific projects to increase our success in this regard.
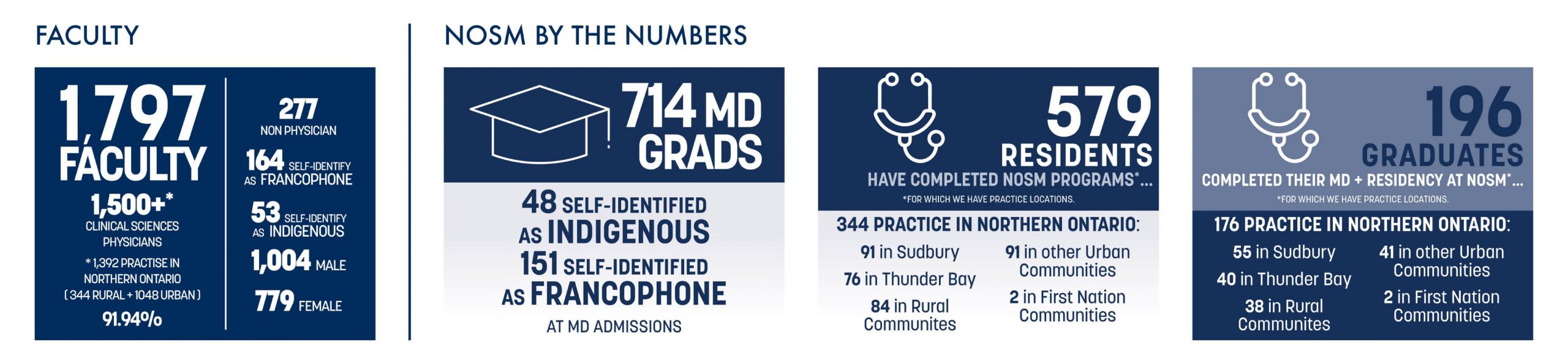
As a government strategy, NOSM has been a success and has obviously had an impact in Northern Ontario. But we can do better and at NOSM we are poised to do so. Check out our new strategic plan at strategicplan.nosm.ca.
Thank you, miigwetch, merci to all.
Please continue to follow my journey on Twitter @ddsv3 using #WhereisDrVerma.
I welcome input on this blog and other issues you want to bring to my attention by email to dean@nosm.ca.
Did you know?
Canada has among the lowest number of practicing physicians per thousand population compared to other OECD countries, ranking 29th out of 33, with a ratio of 2.74/1000 compared to the world average of 3.5/1000. Within Canada, Ontario ranks 8th out of 12 provinces/territories in physician to population ratio. At present, more than 1.3 million Ontarians still do not have regular access to primary care (Stats Canada, 2016).
Did you know?
Dr. Sarah McIsaac, NOSM’s Medical Director, Faculty Development, has partnered with the School on a Crazy Socks for Docs initiative. By making a gift of $20 or more, you will receive a pair of Crazy Socks for NOSM Docs and help us develop programming and support specifically for faculty at NOSM. These past few months have been challenging for everyone, and Dr. McIsaac believes it is important that we create a network of support and inclusivity.
Did you know?
If you are searching for a family doctor, here are a few tips:
Learn how to find a family doctor, nurse practitioner or specialist and details about the Health Care Connect program.
- Register with Health Care Connect and have a nurse find a doctor or nurse practitioner for you.
- Use The College of Physicians and Surgeons of Ontario’s Find a Doctor search. And choose “Advanced Search” to find a doctor near you (by city/town or postal code).
Also, a resource titled We’re Your Family Doctors is recommended by Dr. Sarah Newbery (NOSM’s Assistant Dean, Physician Workforce Strategy and former President of the Ontario College of Family Physicians) is a tool for understanding how to ensure you access your own family doctor if you have one, and how to find other ways to access care if you do not have one yet.
Did you know?
A virtual panel event is being hosted to discuss the benefits of hiring a Physician Assistant to help support your practice and how you can become a clinical partner and offer placements for the PA Program. In the era of COVID-19, and with health system resources being stretched thin, the panel will include those who have supervised student PAs and subsequently hired them. Never has there been a better time to add such a valuable resource to your team.
Wednesday, December 2, 2020
5:00 – 6:00 p.m. EST
RSVP here.
For more information, visit nosm.ca/pa.



