
Preparing to Apply to Medicine….
-
- Get familiar with the Application Information
- Make sure you will meet the Admissions Requirements
- Inventory your skill sets
Dr. Kayla Berst, NOSM Assistant Professor and Alumna, speaks about her NOSM journey.
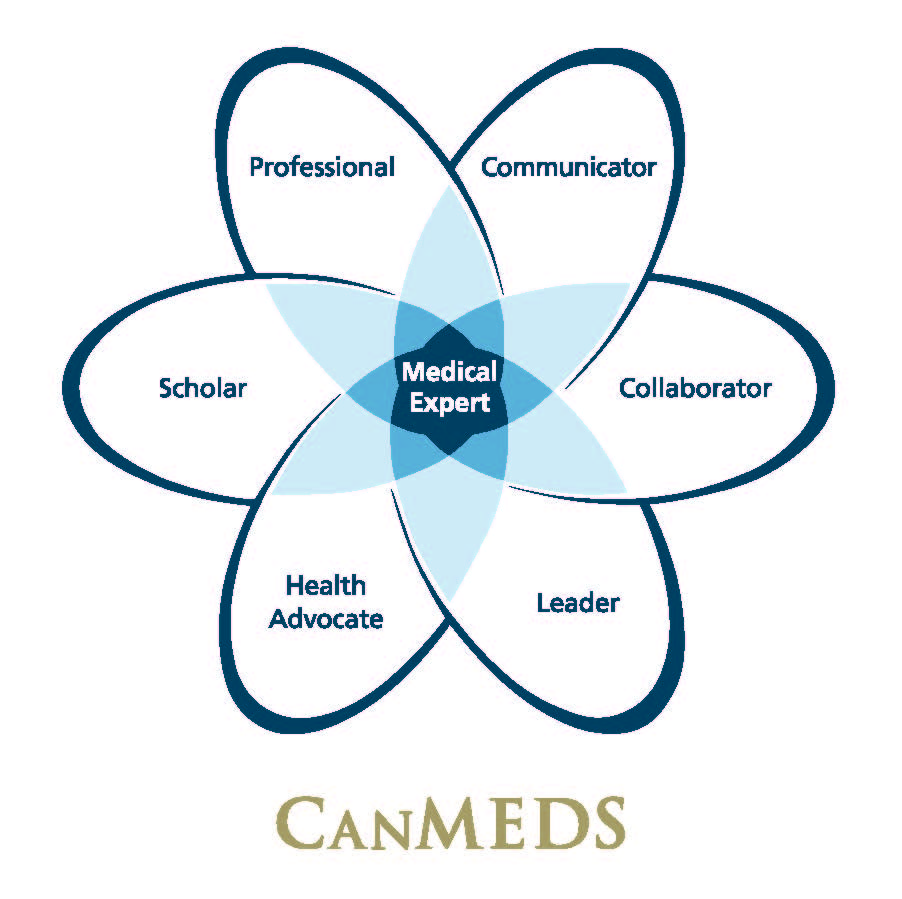
The Royal College of Physicians and Surgeons of Canada has created a framework that identifies and describes the abilities required by doctors to effectively meet the health-care needs of the people they serve.
This framework of abilities is called the CanMEDS Roles, and the NOSM University Admissions process is set up to look for the potential of an individual to develop these skills in those who apply to medicine. So, as you consider what to focus on and what skills you need to develop while you are in university, and/or while you are working or volunteering, consider the CanMEDS Roles.
 Copyright © 2015 The Royal College of Physicians and Surgeons of Canada. Reproduced with permission.
Copyright © 2015 The Royal College of Physicians and Surgeons of Canada. Reproduced with permission.
Medical Expert (the integrating role)
¹Banji F, Lawrence K, Goldszmidt M, Walton M, Harris K, Creery D, Sherbino J, St-Marie L-G, Stang A. Medical Expert. In: Frank JR, Snell L, Sherbino J, editors. CanMEDS 2015 Physician Competency Framework. Ottawa: Royal College of Physicians and Surgeons of Canada; 2015.
Communicator
Because illness affects not only patients but also their families, physicians must be able to communicate effectively with everyone involved in the patient’s care.¹
¹Neville A, Weston W, Martin D, Samson L, Feldman P, Wallace G, Jamoulle O, François J, Lussier M-T, Dojeiji S. Communicator. In: Frank JR, Snell L, Sherbino J, editors. CanMEDS 2015 Physician Competency Framework. Ottawa: Royal College of Physicians and Surgeons of Canada; 2015.
Collaborator
Collaboration requires relationships based in trust, respect, and shared decision-marking among a variety of individuals with complementary skills in multiple settings across the continuum of care. It involves sharing knowledge, perspectives, and responsibilities, and a willingness to learn together. This requires understanding the roles of others, pursuing common goals and outcomes, and managing differences.
Collaboration skills are broadly applicable to activities beyond clinical care, such as administration, education, advocacy, and scholarship.¹
¹Richardson D, Calder L, Dean H, Glover Takahashi S, Lebel P, Maniate J, Martin D, Nasmith L, Newton C, Steinert Y. Collaborator. In: Frank JR, Snell L, Sherbino J, editors. CanMEDS 2015 Physician Competency Framework. Ottawa: Royal College of Physicians and Surgeons of Canada; 2015.
Leader
¹Dath D, Chan M-K, Anderson G, Burke A, Razack S, Lieff S, Moineau G, Chiu A, Ellison P. Leader. In: Frank JR, Snell L, Sherbino J, editors. CanMEDS 2015 Physician Competency Framework. Ottawa: Royal College of Physicians and Surgeons of Canada; 2015.
Health Advocate
Improving health is not limited to mitigating illness or trauma, but also involved disease prevention, health promotion, and health protection. Improving health also includes promoting health equity, whereby individuals and populations reach their full health potential without being disadvantaged by, for examples, race, ethnicity, religion, gender, sexual orientation, age, social class, economic status, or level of education.
Physicians leverage their position to support patients in navigating the health care system and to advocate with them to access appropriate resources in a timely manner. Physicians seek to improve the quality of both their clinical practice and associated organizations by addressing the health needs of the patients, communities, or populations they serve. Physicians promote healthy communities and populations by influencing the system (or by supporting others who influence the system), both within and outside of their work environments.
Advocacy requires action. Physicians contribute their knowledge of the determinants of health to positively influence the health of the patients, communities, or populations they serve. Physicians gather information and perceptions about issues, working with patients and their families* to develop an understanding of needs and potential mechanisms to address these needs. Physicians support patients, communities, or populations to call for change, and they speak on behalf of others when needed. Physicians increase awareness about important health issues at the patient, community, or population level. They support or lead the mobilization of resources (e.g. financial, material, or human resources) on small or large scales.
Physician advocacy occurs within complex system and thus requires the development of partnerships with patients, their families and support networks, or community agencies and organizations to influence health determinants. Advocacy often requires engaging other health care professionals, community agencies, administrators, and policy makers.¹
†In the CanMEDS 2015 Framework, a “community” is a group of people and/or patients connected to one’s practice, and a “population” is a group of people and/or patients with a shared issue or characteristic.
¹Sherbino J, Bonnycastle D, Côté B, Flynn L, Hunter A, Ince-Cushman D, Konkin J, Oandasan I, Regehr G, Richardson D, Zigby J. Health Advocate. In: Frank JR, Snell L, Sherbino J, editors. CanMEDS 2015 Physician Competency Framework. Ottawa: Royal College of Physicians and Surgeons of Canada; 2015.
Scholar
Physicians strive to master their domains of expertise and to share their knowledge. As lifelong learners, they implement a planned approach to learning in order to improve in each CanMEDS Role. They recognize the need to continually learn and to model the practice of lifelong learning for others. As teachers they facilitate, individually and through teams, the education of students and physicians in training, colleagues, co-workers, the public, and others.
Physicians are able to identify pertinent evidence, evaluate it using specific criteria, and apply it in their practice and scholarly activities. Through their engagement in evidence-informed and shared decision-making, they recognize uncertainty in practice and formulate questions to address knowledge gaps. Using skills in navigating information resources, they identify evidence syntheses that are relevant to these questions and arrive at clinical decisions that are informed by evidence while taking patient values and preferences into account.
Finally, physicians’ scholarly abilities allow them to contribute to the application, dissemination, translation, and creation of knowledge and practices applicable to health care.¹
¹Richardson D, Oswald A, Chan M-K, Lang ES, Harvey BJ, editors. Scholar. In: Frank JR, Snell L, Sherbino J, editors. CanMEDS 2015 Physician Competency Framework. Ottawa: Royal College of Physicians and Surgeons of Canada; 2015.
Professional
¹Snell L, Flynn L, Pauls M, Kearney R, Warren A, Sternszus R, Cruess R, Cruess S, Hatala R, Dupré M, Bukowskyj M, Edwards S, Cohen J, Chakravarti A, Nickelle L, WRight J. Professional. In: Frank JR, Snell L, Sherbino J, editors. CanMEDS 2015 Physician Competency Framework. Ottawa: Royal College of Physicians and Surgeons of Canada; 2015.
*Throughout the CanMEDS 2015 Framework and Milestone Guide, references to the patients family are intended to include all those who are personally significant to the patients and are concerned with his or her care, including, according to the patient’s circumstances, family members, partners, caregivers, legal guardians, and substitute decision-makers.
For more information about the CanMEDS Framework visit the Royal College of Physicians and Surgeons of Canada CanMEDS webpage.




